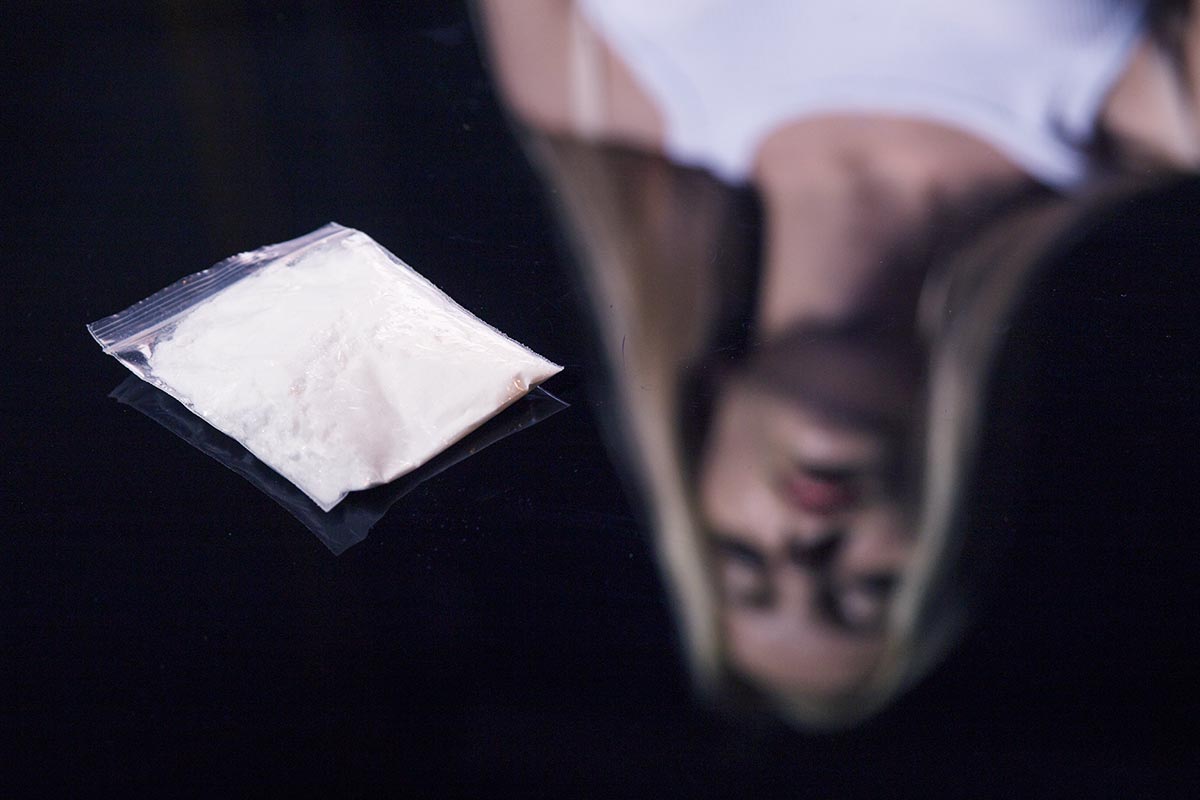
What Is Cocaine Cut With?
 Cocaine is a euphoria-inducing drug often used recreationally in the United States. For many people, cocaine is a casual use drug, which never escalates into a problem or problematic use. In fact, in 2022, over half a million people used cocaine for the first time. For many of those people, cocaine is seen as a relatively safe and low-impact drug that wears off quickly and has few side-effects other than a hangover and maybe a nosebleed or two. At the same time, 1.4 million Americans aged 12 or older (0.5% of the population) also have a substance use disorder or problematic usage of cocaine.
Cocaine is a euphoria-inducing drug often used recreationally in the United States. For many people, cocaine is a casual use drug, which never escalates into a problem or problematic use. In fact, in 2022, over half a million people used cocaine for the first time. For many of those people, cocaine is seen as a relatively safe and low-impact drug that wears off quickly and has few side-effects other than a hangover and maybe a nosebleed or two. At the same time, 1.4 million Americans aged 12 or older (0.5% of the population) also have a substance use disorder or problematic usage of cocaine.
In addition, while millions of Americans will use cocaine and then only use it occasionally, it remains dangerous. Cocaine is a powerful stimulant that causes stress on the cardiovascular system and can result in heart attack or heart problems. In addition, it interacts badly with many other drugs. And, increasingly, cocaine is cut not with potentially illness-inducing white powders but with other, stronger drugs that look similar but cost less to acquire.
As a result, every single time you use cocaine, you could end up in the hospital. Using a drug like cocaine is always a risk. That’s because it’s unregulated, you have no idea what you’re taking, and you could experience negative cardiovascular side-effects that could be fatal.
Why is Cocaine Cut?
Cocaine can be cut for a number of reasons. However, the most common is that the dealer is trying to save money or the person they bought it from is. Here, cocaine is often mixed with white powders that look similar to cocaine, or so much so that you couldn’t tell the difference.
Cocaine can also be cut if what you’re taking is not actually cocaine. For example, it’s increasingly common to see products that are essentially fentanyl powder cut with baby powder or talk sold as cocaine. There’s no actual cocaine in the product, but the dealers often don’t even know that. Instead, they get “cheap” cocaine, which they can then sell for a higher profit margin or pass on cheaply.
In each case, the primary goal is more money for someone in the chain of manufacturer to dealer. And, in some cases, that can result in significant danger to the user, because the person selling the cocaine doesn’t necessarily know what they are selling or what safe usage looks like.
Get Your Questions Answered
What is Cocaine Cut With?
 Cocaine is cut with a large number of substances. The only thing they have in common is that all of them are white powders. Adulterants and cutting agents can include:
Cocaine is cut with a large number of substances. The only thing they have in common is that all of them are white powders. Adulterants and cutting agents can include:
- Flour
- Baking soda/powder
- Baby powder (unscented)
- Talcum
- Boric acid
- Gypsum powder/chalk
These “fillers” increase the quantity of “cocaine” the dealer has to sell. Often, they are used to increase the volume of the cocaine to increase profit margin. In this case, it’s common to see ratios of 10-60% of what are essentially household ingredients used as cutting agents.
However, there are other cutting agents often used. These are typically added in the case that the cocaine has been cut too much and someone could tell that their cocaine isn’t doing anything or that it tastes different. They can also be added in the case that there isn’t any actual cocaine in the product you’re being sold, and the dealer wants to ensure that the drug “does something”.
- Levamisole (veterinary strength dewormer with a similar taste and melting point to cocaine)
- Fentanyl (high strength opioid drug which is available cheaply and is commonly used to create faux cocaine)
- Amphetamines (Used to create a euphoric high similar to cocaine, but more cheaply)
- Caffeine (used to create a high similar to cocaine, but with higher risk of cardiovascular complications)
- Hydroxyzine (antihistamine medication)
If there’s a filler in your cocaine, it’s very likely to be one of these. However, you might also end up with a filler like a local analgesic or painkiller, powdered paracetamol, or a similar filler. These are less common but may still be used to cut cocaine.
Are Fillers Dangerous?
In the best-case scenario, fillers in cocaine can be relatively harmless and merely reduce the strength of whatever you’re taking. For example, it’s not exactly healthy to snort flour up your nose or inject it into your veins, but you’ll probably survive it (although injecting it can cause you to go into shock).
However, many substances that are used to cut cocaine are not safe for taking in any kind of volume. Most are also not intended for use via the membrane layer in the nose or mouth or for injection. This means you can easily reach toxicity with substances that might be safe to take via a pill.
What else? Cutting agents like fentanyl can be extremely strong. If you don’t know what you’re taking, you run the risk of an opioid overdose, without having an overdose reversal agent like Naloxone on hand. Finally, agents like amphetamines can be extremely habit inducing and can result in psychosis, behavioral dependency, cardiovascular problems. Cocaine also penetrates the membrane layer between the brain and the cardiovascular system. It can saturate that layer, drawing other substances with it, and can cause toxicity on its own. In this case, the result is often sudden death.
What Can You Do About Cut Cocaine?
Cocaine is never safe to use on its own. Every time you use it, you take on risks to your health. However, additives and fillers add new layers of risk, because you simply don’t know what you’re taking. For that reason, there are many drug testing organizations in the United States, some of which will test your drugs for free. The best solution is always to not use illicit drugs. However, if you’re going to use them anyway, organizations like DanceSafe provide avenues to ensure that you’re using in as safe of a way as possible. Often, that means ordering drug testing kits or taking a sample of your drugs in to be tested. This won’t get you into trouble. However, you will get a report back on what’s actually in your cocaine, so you can make a decision about whether it’s safe enough for you to use. For example, most people might be surprised to learn that about 5% of all cocaine collected by the DEA includes fentanyl or heroin. Understanding the risks and that you are taking an opioid can allow you to practice much better drug safety.
And, of course, most of us aren’t to pleased with the prospect of using household cleaning products or baby powder as a drug either.
 Getting Help
Getting Help
If you or a loved one is using cocaine, it’s important to understand that it is a risk. For example, in 2022, roughly 10,000 people died of stimulant-related overdose without contaminants like fentanyl and a further 47,000 died of overdose-deaths after taking a stimulant mixed with fentanyl or heroin.
Many people see cocaine as a safe drug that they can use and have vanish in a few hours. While that’s often the case, the drug comes with its own significant risks and it’s never safe to use, even if you’ve safely used it before. That may mean it’s important to get help, to look into talking to your doctor about drug use, and to get treatment or therapy to explore the reasons behind using, so you can improve those direct causes and not need it.


 Cannabis can temporarily relieve head pain and muscle pain by relieving inflammation. However,
Cannabis can temporarily relieve head pain and muscle pain by relieving inflammation. However, 


 Meth and crack cocaine have a lot in common. For example, they are both stimulant drugs. This means that both impact the central nervous system causing a high, euphoria, and feelings of being powerful. People using crack or meth will show signs of hyperactivity, wakefulness, and restlessness. They might not be able to sit still, talk at a normal pace, or they might talk with nervous energy or jitters.
Meth and crack cocaine have a lot in common. For example, they are both stimulant drugs. This means that both impact the central nervous system causing a high, euphoria, and feelings of being powerful. People using crack or meth will show signs of hyperactivity, wakefulness, and restlessness. They might not be able to sit still, talk at a normal pace, or they might talk with nervous energy or jitters.
 Cocaine
Cocaine
 You’ll have to set boundaries with your partner, decide if you want to stay with them, and decide if you can even be fair to them in a relationship. Before you do, you should figure out answers to questions like:
You’ll have to set boundaries with your partner, decide if you want to stay with them, and decide if you can even be fair to them in a relationship. Before you do, you should figure out answers to questions like: Talk to Your Loved One
Talk to Your Loved One Taking time to understand addiction, how it works and what help looks like is important if you want to stay with your partner. Even if you’re casually dating, you’ll want to know what addiction is and what treatment looks like. That means taking time to
Taking time to understand addiction, how it works and what help looks like is important if you want to stay with your partner. Even if you’re casually dating, you’ll want to know what addiction is and what treatment looks like. That means taking time to